Top 5 Signs Your Practice Is Missing Collections

Revenue Leakage Audit Worksheet
Download the complete audit worksheet with benchmarks to find the $25K-$50K your practice loses annually.
Most practices losing money do not realize it until the damage is done. These warning signs tell you to look deeper before it is too late.
📚 Part of our reconciliation series: This article is part of The Complete Guide to Dental Practice Reconciliation, our comprehensive resource on closing your books accurately and preventing revenue leakage.
The Silent Revenue Drain
Dental practices lose revenue every day without knowing it. The losses are small enough to miss in daily operations but significant enough to matter over months and years. A missed insurance payment here. An unposted check there. A patient who walked out without paying.
These small leaks add up. A practice collecting one million dollars annually might lose twenty-five to fifty thousand dollars through preventable gaps. The money is not gone because of fraud or theft. It simply fell through operational cracks that nobody noticed.
These five warning signs indicate your practice may be losing revenue. If you see any of them, investigate immediately.
Sign 1: Unidentified Deposits Keep Growing
Your bank shows deposits that your practice management system cannot explain. When you ask who paid, nobody knows. When you try to match deposits to patient payments, some do not match anything.
A small unidentified deposit balance is normal as recent deposits await matching. A large or growing balance is a warning sign indicating that insurance EFTs are depositing without ERA matching, checks are being deposited without proper posting, combined deposits are not being broken down, or payments are being received that your PMS does not know about.
Every dollar in unidentified deposits is a dollar not credited to the patient who paid it. Those patients may get billed again, creating patient service issues. Or the money may eventually be written off as unidentifiable income.
What to do: Require that every deposit be matched to specific payments within forty-eight hours. Research and resolve the existing unidentified balance. Establish a maximum acceptable unidentified deposit level and investigate when it is exceeded.
Sign 2: Collection Rate Is Below Ninety-Five Percent
Net collection rate measures how much you actually collect versus how much you should collect after contractual adjustments. A healthy practice collects ninety-five percent or more.
Below ninety-five percent indicates systematic collection problems. Patients are leaving without paying their portions. Insurance payments are not being followed up. Claims are being denied without appeal. Adjustments are being made that should not be.
Collection rate below ninety percent is serious. Below eighty-five percent is a crisis requiring immediate intervention.
What to do: Calculate your actual collection rate for the past six months. If it is below target, dig into the components. Are patient collections weak? Is insurance follow-up insufficient? Are adjustments excessive? Address each problem area systematically.
Sign 3: AR Over Ninety Days Exceeds Fifteen Percent
Accounts receivable aging shows how long balances have been outstanding. Fresh AR, meaning under thirty days, is normal. Aged AR, meaning over ninety days, is often uncollectible.
When more than fifteen percent of your AR is over ninety days old, you are carrying balances that will likely never be collected. Those balances inflate your reported AR, masking the true financial picture.
Excessive aged AR indicates insurance claims are not being worked, patient statements are not being sent, collection efforts are not escalating appropriately, and old balances are not being written off when truly uncollectible.
What to do: Review your AR aging report. Identify the largest aged balances and research each one. Work everything that is workable. Write off what is truly uncollectible. Establish AR management processes that prevent future accumulation.
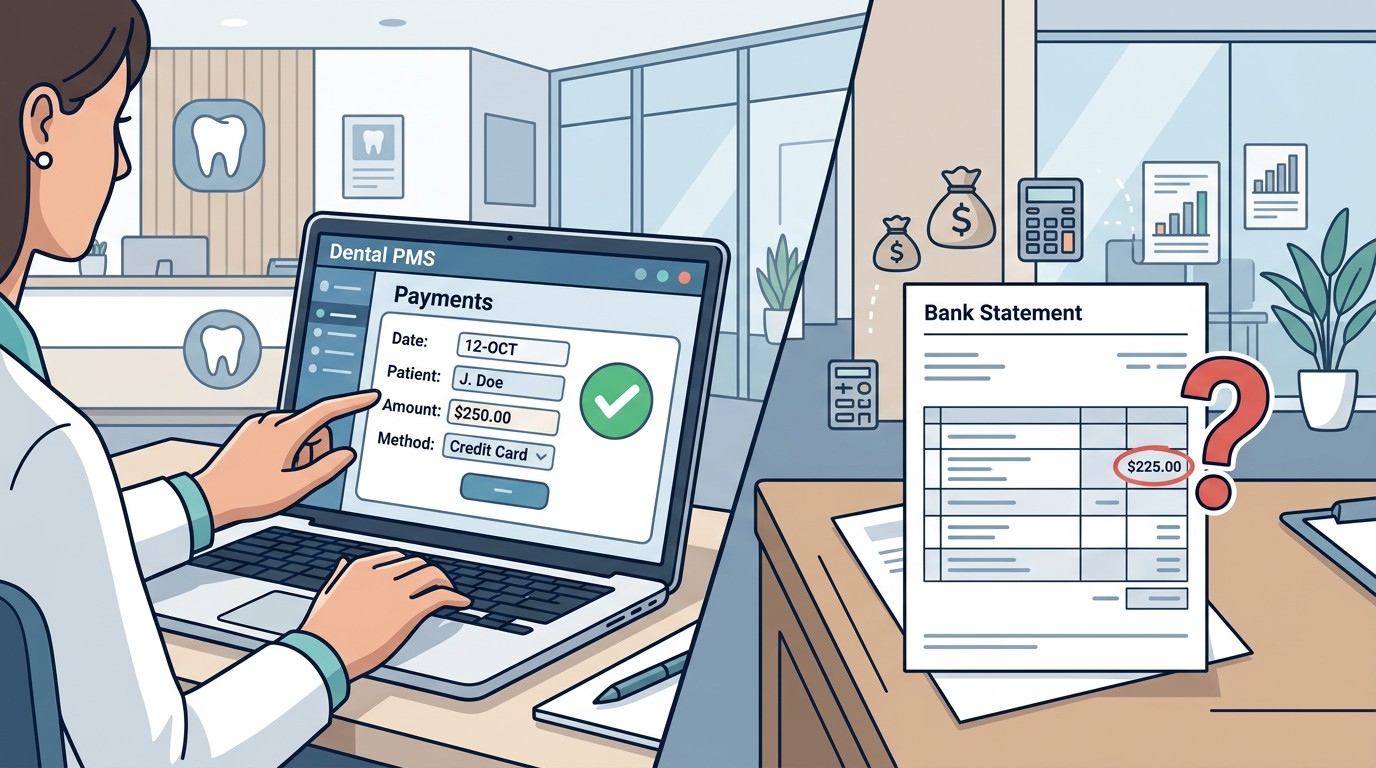
Sign 4: Day Sheet Totals Never Match Deposits
At the end of each day, your PMS shows what was collected. The next day, deposits hit your bank. These numbers should match.
When they consistently do not match, something is wrong. If PMS exceeds deposits, payments are being recorded but not actually collected or deposited. If deposits exceed PMS, payments are being collected but not recorded.
Either direction indicates control breakdown. The first scenario suggests posting errors or potential theft. The second suggests unposted payments and patients not getting credit.
What to do: Compare your day sheet totals to actual bank deposits for the past month. Calculate the variance rate. If it exceeds two to three percent, investigate the causes. Implement daily reconciliation that catches and resolves variances same-day.
Sign 5: Nobody Can Explain the Adjustments
Adjustments reduce revenue. Some adjustments are necessary and appropriate, including contractual adjustments for insurance discounts. Others should be questioned, including write-offs for unclear reasons.
When nobody can explain why adjustments were made, control has broken down. Staff may be writing off balances to avoid difficult collection conversations. Errors may be hidden through adjustments rather than corrected properly. Theft may be concealed through false adjustments.
What to do: Review all adjustments for the past month. Verify each has an appropriate reason code. Question any adjustment that lacks clear documentation. Establish approval requirements for adjustments above certain thresholds.
Taking Action
If you see one warning sign, investigate that specific area. If you see multiple warning signs, you have a systemic problem requiring comprehensive review of your revenue cycle.
Do not wait for year-end to discover you have been losing money all year. Check for these signs monthly. Catch problems early when they are still small and correctable.
Worried about missing collections? Zeldent monitors your revenue cycle daily, flagging these warning signs automatically. Schedule a demo to see where your revenue goes.
Revenue Leakage Audit Worksheet
Download the complete audit worksheet with benchmarks to find the $25K-$50K your practice loses annually.