What Is Dental Revenue Leakage? Causes, Examples, and Fixes
Revenue Leakage Audit Worksheet
Download the complete audit worksheet with benchmarks to find the $25K-$50K your practice loses annually.
Dental revenue loss is a quiet problem - it is money a practice earns but does not collect. The loss hides in billing mistakes, slow insurance payments, data entry errors, or poor follow up. For practice owners and office managers, the challenge is that the loss does not always show clearly in financial reports. It quietly decreases profit month after month.
📚 Part of our reconciliation series: This article is part of The Complete Guide to Dental Practice Reconciliation, our comprehensive resource on closing your books accurately and preventing revenue leakage.
The article defines revenue loss in dentistry. It explains common causes and shares examples - it offers proven ways to fix the problem. You will learn practical ways to protect your revenue, improve billing accuracy, and strengthen cash flow. By the end, you will know how to find loss, measure its effect along with stop it from happening again.
Understanding Dental Revenue Loss
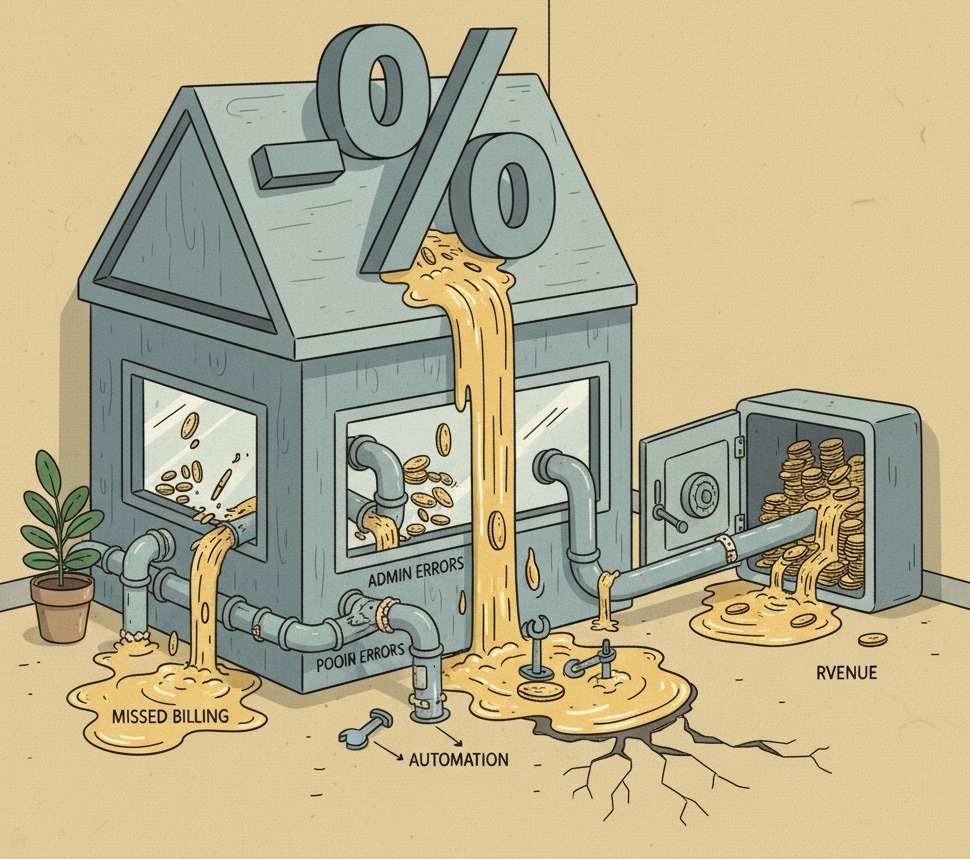
Revenue loss is the income a practice does not collect. It happens because of process faults, errors, or oversight. In dentistry, this often includes claims a payer denies, incorrect codes, services a practice does not bill, patient payments a practice misses, or old accounts receivable - it is not production a practice loses, but money earned that a practice never deposits into the bank.
Why It Matters
Revenue loss affects profit, team spirit in addition to patient satisfaction. When collections slow, cash flow gets tight. This causes stress on payroll, investments in new equipment, and the overall financial stability of the practice. Even a small percent of loss, when added up over a year, can mean tens or hundreds of thousands of dollars a practice loses. A practice that consistently loses 10 percent of its revenue works more for less.
The Cost of Hidden Loss
Industry studies show that practices lose between 5 and 20 percent of their production each year to revenue loss. For a practice making $100,000 a month, that could mean between $60,000 and $240,000 each year. The problem is not that a practice did not deliver the services. The problem is that a practice never gets the payment. Because the losses often happen in small amounts, they can go unnoticed until they become a very big problem.
Common Causes of Revenue Loss in Dental Practices
Incorrect codes, outdated CDT updates, or mismatched procedure codes often cause claim denials. Even when a practice fixes them later, the errors slow down collections and increase costs. As an example using an outdated CDT code for a common procedure may lead to months of going back and forth with the insurer. Training staff and staying current with coding updates is very important to stop this form of loss.
Denied or Delayed Claims
Insurance carriers deny claims for many reasons. Some of the most common include missing paperwork, incorrect items like X-rays, eligibility errors, or issues with coordination of benefits. Each denied claim requires rework, resubmission next to tracking. Without careful follow up, a practice can forget the claims and eventually write them off. A practice with many denied claims leaves earned money uncollected.
Data Entry Mistakes and Patient Information Errors
A simple mistake in a date of birth, insurance ID, or policy number can cause a claim rejection. Front desk and billing staff need to check patient information at registration. Accuracy at the start prevents costly errors later in the revenue cycle. One missed digit in an insurance number can cause dozens of claims to bounce back.
Poor Accounts Receivable Management
When a practice does not follow up on accounts receivable within 30 to 60 days, the chance of recovery drops a lot. Practices that let balances age past 90 days often write off revenue a practice should have collected. A common mistake is to think small balances are not worth the effort, but together, they add up to thousands over the year.
Inefficient In-House Billing
Handling billing inside the practice can seem like a way to save money. It often introduces hidden costs. Staff changes, lack of training, other work duties can lead to delays and errors. As an example, a front desk coordinator who handles scheduling and billing may prioritize urgent patient needs over collections follow up. Using outside help or adding specialized billing support often improves collections and reduces loss.
Multi-Location Coordination Failures
For group practices or DSOs, differences across locations create loss. Each office may have its own billing processes, KPIs along with reports. Without standardization, leadership cannot see where loss is happening or how to fix it. One office may collect 96 percent while another operates at 85 percent, but without centralized reporting, those differences remain hidden.
Lack of Eligibility Verification
Failure to check patient insurance eligibility before treatment is another major cause of loss. Practices that skip real time eligibility checks risk providing services that a payer later denies - this leaves balances uncollectible. Patients are often surprised by costs that their plan does not cover, which increases tension and reduces payment likelihood.
Uncollected Patient Balances
Patients leaving without paying co pays or deductibles create immediate loss. Without card-on-file systems or strict financial policies, practices often chase the balances for months. Many balances are never recovered.
Examples and Real-World Effect
A mid sized practice making $80,000 a month found during an audit that it had not collected $120,000 of insurance claims over two years. The claims were denied at first because of missing attachments. A practice never followed up on them. That oversight represented nearly 8 percent of lost production.
Example - Understaffed Billing Teams
A single office manager handling front desk, scheduling in addition to billing could not keep up. Claims piled up. Accounts receivable aged past 90 days. Write-offs increased. Hiring a part time billing specialist helped recover $50,000 in the first six months.
Example - Data Errors
In one case, a payer denied many claims because staff entered incorrect insurance ID numbers. The errors added up over time causing patient frustration and revenue loss. After adding a double check system at registration, denials dropped a lot.
Example - Inconsistent Multi-Office Processes
A DSO with five locations found that each office had different billing protocols. Some required insurance verification. Others did not. The result was inconsistent collections across the group. One office lost nearly 15 percent of its revenue to loss compared to 6 percent at another.
Fixes - Preventing and Recovering from Leakage
Automation reduces manual entry - it also finds errors early. Clean claim scrubbing, automated eligibility checks, and electronic claim submission increase collections. The actions also reduce denials. Practices which use automation see denial rates drop by 30 to 40 percent.
Centralize Billing and Coding
For multi location practices centralizing billing shows consistency. A single team which manages coding and claims across offices applies standard processes. This reduces variation which causes problems. Centralization also lets leadership see overall performance.
Train and Cross-Train Staff
Every staff member who handles patient information or billing needs training on precision and compliance. Cross-training shows that revenue processes continue even if one employee is absent or leaves the practice. Practices with well trained, flexible teams have fewer delays and fewer problems.
Monitor Important Billing KPIs
Track metrics such as clean claim rate, denial percentage, collections percentage, and A/R aging by type. Monitoring the KPIs weekly lets you see problems before they become big. A sudden rise in denial percentage, for example, signals a coding or data entry issue.
Audit and Adjust Systems Regularly
Conduct monthly small audits. Conduct quarterly full audits. Review a sample of claims from start to finish to show precision. Look for repeated errors. Adjust work processes. Auditing builds resilience into your systems.
Strengthen Patient Collection Policies
Require co-pays and deductibles at the time of service when possible. Use card-on-file systems. Offer payment plans to reduce unpaid balances. Clear communication about financial duty builds trust. It also reduces surprises.
Improve Communication Between Clinical and Billing Teams
Sometimes revenue problems happen because clinical notes are incomplete. Or they do not communicate well to billing staff. Encourage regular meetings between clinicians and billers - this shows that all procedures are coded correctly and supported by documents.
A Useful Insight - Visualizing Revenue Leakage
Numbers in spreadsheets appear abstract. Visualization tools such as dashboards show leakage to teams. Showing staff how much money is at risk, or how collections improve after fixes, creates accountability and motivation. Practices which show leakage often see faster adoption of correct habits. A dashboard which shows “dollars at risk” compared to “dollars collected” is a really powerful motivator.
The Future of Revenue Protection
AI-driven billing software predicts claim denials before submission - it flags errors based on past information. That lets teams correct issues before the claim reaches the insurer. It improves first pass acceptance rates.
Benchmarking Across DSOs
Large groups benchmark revenue cycle KPIs across offices; they see which locations have the best performance. They copy those processes. Smaller practices apply the same idea by comparing month-over-month performance.
Increased Focus on Compliance
Regulators place more review on healthcare billing. Compliance-driven work processes are not just about avoiding penalties - they are also about showing revenue integrity. A compliant practice is a more profitable practice.
Quick Takeaways
- Revenue leakage is income earned but never collected because of errors or issues.
- Common causes include coding mistakes, denied claims, patient data errors, poor A/R follow-up along with inconsistent processes.
- Practices lose between 5 and 20 percent of production annually from leakage.
- Solutions include automation, centralized billing, staff training, strict patient policies, and KPI monitoring.
- Visualization and audits help make revenue leakage visible and fixable.
- The future will rely on AI, benchmarking in addition to compliance-driven processes.
Conclusion
Revenue leakage in dental practices appears invisible at first glance. But its impact is clear and costly. Lost claims, delayed collections next to billing errors add up to quite large financial drains. The good news is that once identified, most leaks stop with structured processes, modern technology, regular oversight.
For owners and office managers, the priority is to build a culture of precision and accountability. Automating the revenue cycle centralizing billing when possible training staff well along with monitoring KPIs are proven ways to protect income. Every leak plugged is not just money saved, but money earned. That revenue then reinvests in new technology, better staff support, or expanded services.
Do not let hidden leaks undermine your hard work. Take time this month to review your processes, audit your claims in addition to visualize your revenue health. The effort you put in now translates into tens of thousands of dollars back in your practice every year.
Revenue Leakage Audit Worksheet
Download the complete audit worksheet with benchmarks to find the $25K-$50K your practice loses annually.